Publication: Impaired high-density lipoprotein function in patients with heart failure
In a study by Lisa Emmens and Congzhuo Jia et al. published in Journal of the American Heart Association, it was shown that a better high-density lipoprotein (HDL) cholesterol efflux capacity was associated with a lower risk of mortality in heart failure. In addition, it was observed that HDL cholesterol efflux and anti-inflammatory capacity of HDL declined during follow-up in patients with heart failure after initial presentation with new-onset or worsening heart failure. Other members from Groningen Cardiology involved in this project included Rudolf de Boer, Adriaan Voors, and Dirk Jan van Veldhuisen.
Recently, HDL cholesterol was found to be among the strongest predictors of death and/or hospitalization for heart failure in two large European heart failure cohorts. In addition, low concentrations of HDL cholesterol have previously been associated with a higher incidence of heart failure, and with worse outcomes in patients with established heart failure. However, HDL cholesterol-increasing therapies have failed to show clear benefit, which has cast doubt on whether HDL, as conventionally measured, can be ascribed a causal protective role.
Three measures of HDL function
HDL has a high proteomic complexity and a wide range of biological effects, which are not captured by simply measuring conventional HDL cholesterol concentrations. Therefore, in this study, HDL functionality was investigated according to three measures of HDL function: HDL cholesterol efflux, anti-oxidative capacity, and anti-inflammatory capacity. This was performed in 446 patients from the index cohort of BIOSTAT-CHF, a large European investigator-driven clinical study. HDL functionality was measured at initial presentation of new-onset or worsening heart failure and repeated after 9 months. During the time in between, investigators were encouraged to uptitrate heart failure medication in their patients. HDL functionality was furthermore linked to HDL proteome content in 86 patienst from BIOSTAT-CHF.
Main findings
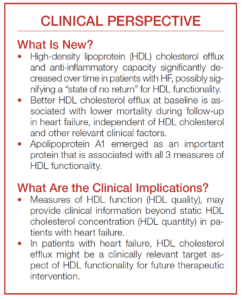
The main findings of this study were, firstly, that a better high-density lipoprotein (HDL) cholesterol efflux at baseline was associated with a lower risk of mortality in heart failure, independent of HDL cholesterol and other relevant clinical factors. Secondly, HDL cholesterol efflux and anti-inflammatory capacity of HDL significantly decreased over time in patients with heart failure, which could possibly signify a “state of no return” for HDL functionality after initial presentation with new-onset or worsening heart failure. Thirdly and finally, Apolipoprotein A1 emerged as the main protein that was associated with all three measures of HDL functionality.
Measures of HDL function (HDL quality) may thus provide clinical information beyond static HDL cholesterol concentration (HDL quantity) in patients with heart failure.